What is the nocebo effect?
A lot is known about the placebo effect - when sham treatments such as sugar pills induce a positive change in patients or reduce a medical problem’s intensity. The placebo effect is a non-specific part of a treatment where psychological factors like expectations and past experiences trigger a positive change. However, much less is known about the placebo’s counterpart called the Nocebo Effect.
The Nocebo Effect refers to a negative change or worsening of symptoms induced by a placebo or active treatment. For example, a sugar pill prescription for a headache may worsen the headache or induce body aches. The Nocebo Effect can turn into a costly burden for doctors, patients, and insurers – notably, lowered trust between doctors & patients and the economic burden of multiple consultations.
 Blog posts
Blog posts Newristics
Newristics
 18 February 2021
18 February 2021





 Back
Back Share
Share








 Webinars
Webinars
 Video
Video
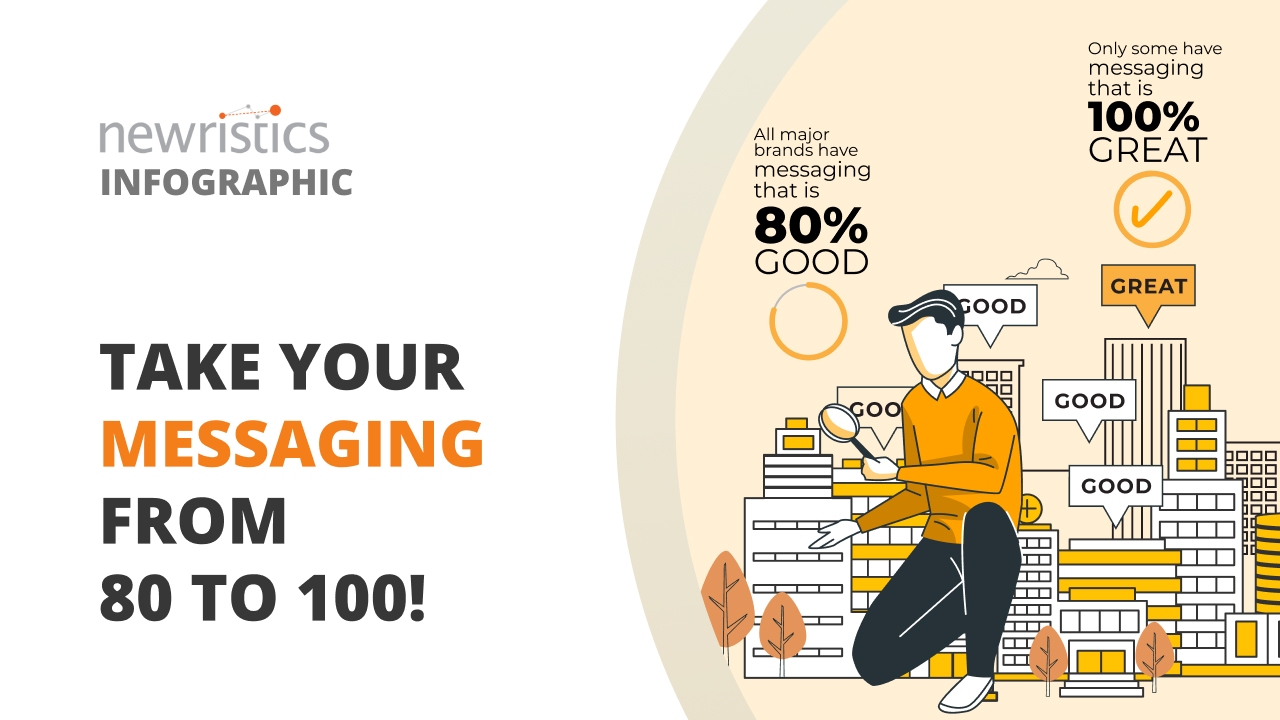
 Infographics
Infographics



